Prostate Biopsies Could Be Avoidable With MRIs: Study
Umer Jamshaid Published January 20, 2017 | 09:25 AM
PARIS, , (APP - UrduPoint / Pakistan Point News - 20th Jan, 2017 ) - A quarter of men suspected of having prostate cancer could avoid invasive and potentially dangerous biopsies with the help of MRI scans, researchers reported Friday.
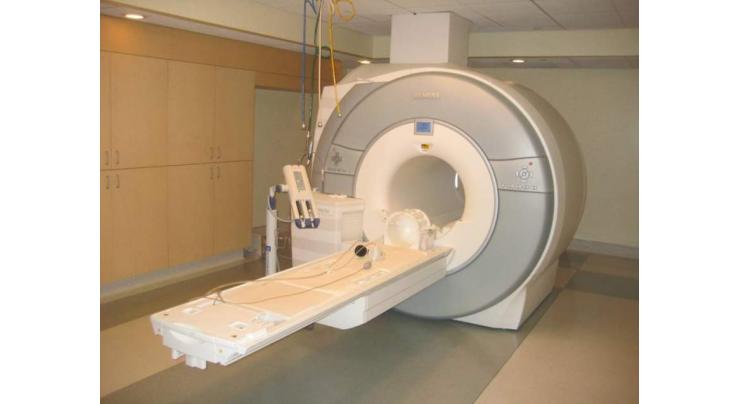
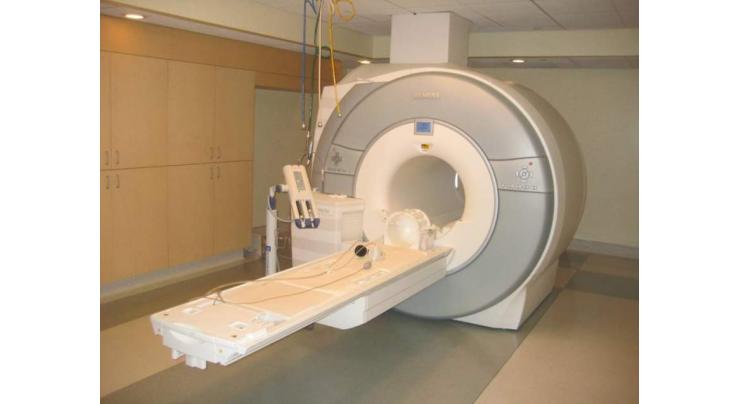
Magnetic resonance imaging (MRI) could also reduce the number of men over-diagnosed with the disease by five percent, they detailed in a study published in The Lancet. The new approach is potentially a game-changer, experts commenting on the study said.
In the case of prostate cancer, "over-diagnosed" includes relatively benign cancers that do not cause any harm during a man's lifetime. "Prostate cancer has aggressive and harmless forms," noted lead author Hashim Ahmed, a surgeon at University College London's faculty of medicine.
Typically, men undergo a prostate biopsy if they experience certain symptoms or show high levels of a protein in their blood, as detected by a prostate specific antigen (PSA) test. Each year, over a million prostate biopsies are done in Europe alone.
The procedure -- which can cause bleeding, pain and serious infections -- involves using a biopsy needle to draw a tissue sample through a small cut made between the anus and scrotum. The needle goes in "blind," and can thus bypass a cancerous mass.
"Our current biopsy test can be inaccurate because the tissue samples are taken at random," Ahmed said in a statement. "It can miss aggressive cancers that are actually there." And if the biopsy does finds cancer cells, it cannot reliably determine whether they are malignant.
As a result, some men are given a false diagnosis and prescribed treatments with nasty side effects. Ahmed and his team wanted to find out if a MRI scan could be used as a "triage" test to determine which men with elevated protein counts might safely avoid a biopsy.
A multi-parametric MRI (MP-MRI) can provide information about a cancer's size, density, and proximity to the bloodstream.
Recent Stories

HEC reviews curricula for environmental sciences degree programme

ICC Asia looking forward to an action-packed Asia Cricket Week

Yuvraj Singh named ICC Men’s T20 World Cup 2024 Ambassador

Greece hands Olympic flame to 2024 Paris Games hosts

Two Kyiv hospitals evacuating over feared Russian strikes

World must act on neurotech revolution, say experts

Charles & Catherine's cancer diagnoses

Champions Alcaraz and Sabalenka through in Madrid Open

King Charles to resume some public duties during cancer treatment: palace

US defense chief announces $6 bn in security aid for Ukraine

Heavy rains cause damage to Spezand-Taftan railway track

Woman stabbed in Israel, attacker killed: police
More Stories From World
-
NFL will allow players to wear Guardian Cap helmets in games
3 hours ago -
Football: German Bundesliga table
3 hours ago -
Football: Italian Serie A result
3 hours ago -
Football: German Bundesliga results
3 hours ago -
US troops to leave Chad in second African state withdrawal
3 hours ago -
Plastics pollution may be solved without production cap: Canada minister
3 hours ago
-
Biden stalls on menthol cigarette ban fearing Black vote backlash
3 hours ago -
Champions Alcaraz and Sabalenka through in Madrid Open
3 hours ago -
6,000 French police to welcome Olympic torch amid bonus boost
4 hours ago -
Taiwan hit by several quakes, strongest reaching 6.1-magnitude
4 hours ago -
'Ballistic' Bairstow stars as Punjab pull off record T20 chase
4 hours ago -
Tennis: ATP/WTA Madrid Open results - 2nd update
4 hours ago